About This Constellation ShortList™
Benefits are becoming more of a strategic compensation asset for enterprises. In a tight talent market, the availability, depth and breadth of benefits can be key for employment decisions and important for keeping attrition low. The enrollment, however, remains a challenge for almost all employees, with their yearly enrollment decisions having deep repercussions affecting their own and their dependents’ lives for the next year or even years to come. At the same time, employee cost is on the rise and benefits are becoming a substantial part of the employee cost.
Ease of enrollment, especially from mobile platforms, is key, while allowing benefits admins to easily create the enrollment experience. Reflecting the global pandemic, vendors need to rethink the way how benefit funds are allocated and what the effectiveness of single benefit offerings is.
To be a benefits administration vendor, these companies need to provide regular innovation on the ease of enrollment. At the same time, they must support the benefits administrator and help turn the tables on the information war on healthcare/services providers. Moreover, they need to have out-of-the box interfaces with the leading HCM suites (see the Constellation ShortLists for Global HCM Suites and North American SMB Payroll) to help enterprises integrate and go live with ease. Listed companies must have 500+ customers in North America, and ideally support for more continents for global benefits. Key new capabilities added in 2020 are for benefits usage and dashboards.
Threshold Criteria
Constellation considers the following criteria for these solutions:
- Enrollment capability
- Mobile enrollment
- Continuous improvement of the enrollment experience
- At least some leverage of AI to assist decision making in the enrollment process by 2023 enrollment
- Easy setup of enrollment mechanics by benefit admins
- At least six of the following areas:
- Explanation capability of benefits decisions
- Ability to simulate enrollment decision consequences
- Low-code/no-code options to augment the enrollment experience
- Interfaces to popular HCM suites
- Enrollment reminders, progress and communications
- Usage and consumption analytics
- Benefit design input and capabilities
- Compliance reporting
- Analytics that reflect the post pandemic needed effectiveness of benefits offerings
- Benefits usage and prediction of usage capabilities
- Powerful dashboard to understand benefits usage and enrollment status
- At least a plan for enabling the benefits guide with generative AI.
- Support for more than one continent
- Over 900 customers and more than 200.75 million benefits enrollment users
- Mobile enrollment version with at least 1,200,000+ users
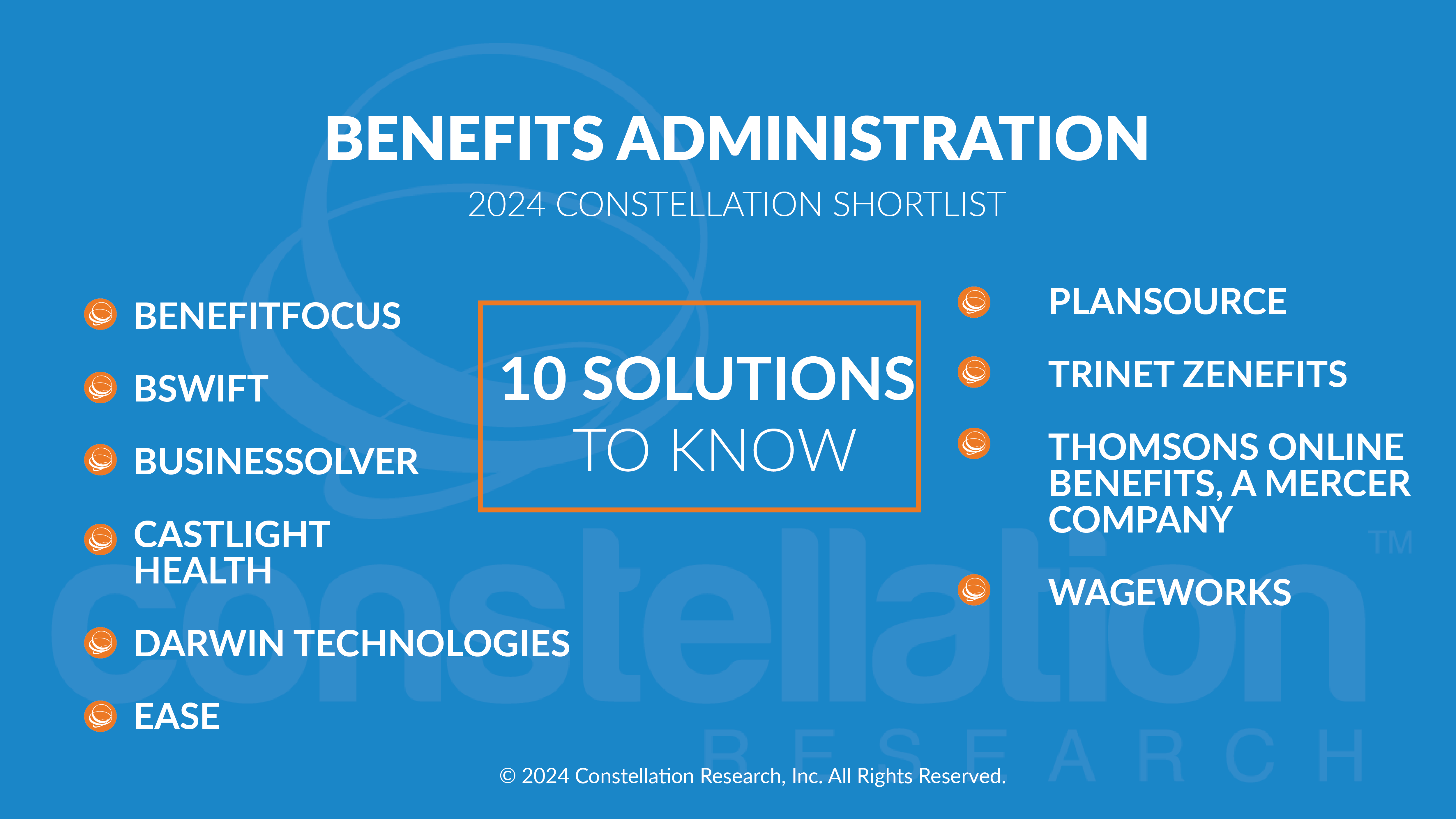
The Constellation ShortList™
Constellation evaluates more than 20 solutions categorized in this market. The Constellation ShortList is determined by client inquiries, partner conversations, customer references, vendor selection projects, market share and internal research.
- BENEFITFOCUS
- BSWIFT
- BUSINESSOLVER
- CASTLIGHT HEALTH
- DARWIN TECHNOLOGIES
- EASE
- PLANSOURCE
- TRINET ZENEFITS
- THOMSONS ONLINE BENEFITS, A MERCER COMPANY
- WAGEWORKS
Frequency of Evaluation
Each Constellation ShortList is updated at least once per year. Updates may occur after six months if deemed necessary.
Evaluation Services
Constellation clients can work with the analyst and the research team to conduct a more thorough discussion of this ShortList. Constellation can also provide guidance in vendor selection and contract negotiation.


