The impacts from a Feb. 21 Change Healthcare ransomware attack continue to be felt as physicians still cannot file claims in many cases and practices are beginning to feel the squeeze.
Change Healthcare, which is owned by UnitedHealth Group, was hit with a ransomware attack that disconnected systems. Change Healthcare processes claims and other financial processes and was attacked by ALPHV/Blackcat.
As Constellation Research analyst Chirag Mehta noted, this ransomware attack had a real impact at the human level. Prescriptions couldn't get filled and physician practices are running out of cash. The American Medical Association issued a letter to the US Department of Health and Human Services to ensure practices can continue to function.
The AMA said in a letter to HHS Secretary Xavier Becerra:
"The cybersecurity incident that has impacted Change Healthcare and resulted in disruptions in claims processing, eligibility checks, and other impacts on day-to-day practice operations that has severely hampered physicians’ ability to care for patients..."
"The AMA is concerned about the undue financial hardships facing physician practices if this incident is not resolved quickly. It is especially challenging financially at the beginning of the year since many practices do not carry over reserves. We are particularly concerned about small, safety net, rural, and other less-resourced practices that often serve underserved patient communities. We urge HHS to utilize any available emergency funds and authorities to provide critical financial resources to physicians, ensuring they can continue to deliver essential health care services during these challenging times."
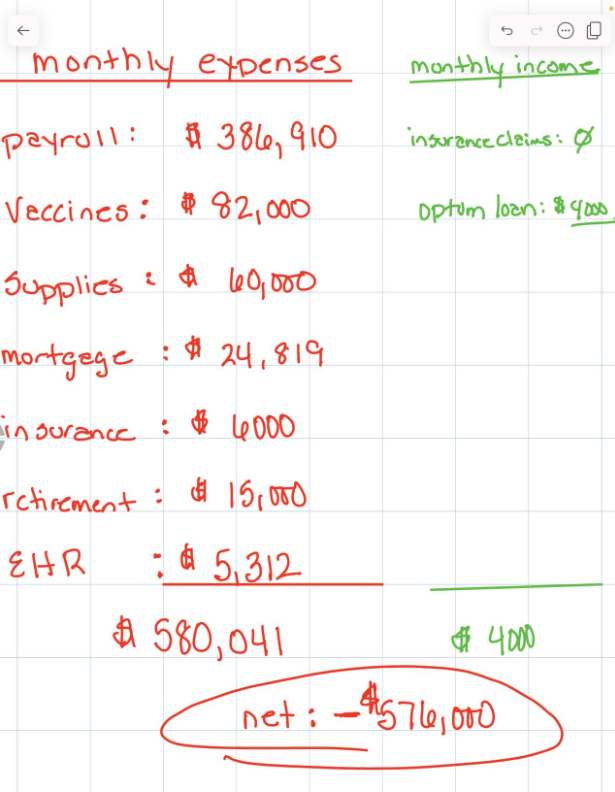
Christine Meyer, MD, a physician with her own practice based in Exton, PA, outlined the pain from the Change Healthcare attack on LinkedIn. She noted that Optum/UnitedHealth Group is providing a $4,000 bridge loan but without the ability to submit bills her practice, which has 84 employees, is running out of cash.
Meyer is also an example of the admin burden that the AMA is also complaining about.
UnitedHealth Group has said it is working with Mandiant and Palo Alto Systems to remediate the ransomware damage and "patient care is our top priority, and we have multiple workarounds to ensure people have access to the medications and the care they need." The company also added links for funding options.
Optum, UnitedHealthcare and UnitedHealth Group systems are unaffected, according to the company. However, it was noted in feedback to Meyer's post that those systems aren't helping much. And UnitedHealth Group's workarounds are a burden. The burden briefly can be found on this FAQ:
"Change Healthcare recommends that providers use the applicable payer’s portal to check claim status, as well as complete eligibility verifications and prior authorizations. If a portal is not available, the recommended approach is calling the appropriate payer’s provider service line."
In its letter, AMA blasted those workarounds.
Practices are being instructed to use direct data entry and portals to submit claims, which are quite labor-intensive compared with using their regular practice management systems that prepopulate data. These “workarounds” are adding extensive administrative burdens as well as substantial costs to physician practices for this extra manual work. In addition, practices are filing claims on paper when available, but many insurance companies no longer accept paper claims."
AMA also said HHS needs to prod Change Healthcare to be more transparent with communication. For now, UnitedHealth Group doesn't have a timeline on when Change Healthcare's systems will return.
"We will not take shortcuts or any additional risk when it comes to safeguarding our information, customer and consumer information, or the connectivity back to our systems. Our systems remain offline because of our diligence, not because of compromise. They will remain offline until we are certain we can turn them back on safely. We took action so you did not have to disconnect."
UnitedHealth completed the acquisition of Change Healthcare in 2022 after winning in court against the US Justice Department, which was against the deal due to antitrust concerns. UnitedHealth's Optum unit said the Change Healthcare can achieve "a simpler, more intelligent and adaptive health system for patients, payers and care providers."
More healthcare:
- Themes from the healthcare data, AI, disruption front lines
- 8 takeaways from Constellation Research's Healthcare Transformation Summit
- Medtronic aims to leverage medical device data for AI-enabled care
- Oracle's plan for Cerner: Cloud shift, generative code rewrite
- CVS Health’s Transformation Rides on Data, AI and Customer Experiences


